Introduction: The primary goal of therapy for polycythemia vera (PV) is the prevention of thrombotic events (TE). Several studies conducted in the United States and Europe have indicated that elevated hematocrit (HCT) and white blood cell count (WBC) are associated with an increased risk of TE in patients with PV. However, these associations have not been reported in Japanese patients with PV.
In this study, we aimed to evaluate the association between blood cell counts and TE in Japanese patients with PV using a real-world database.
Methods: This retrospective cohort study was performed using the RWD database (Real World Data Co., Ltd) which is a large-scale electronic medical records database collected between 1987 and 2022. Patients who met the following criteria were included: 1) PV (ICD-10, D45) initially diagnosed at ≥18 years of age (index date is the date of initial diagnosis); 2) at least one hospital visit within 180 days after the index date; 3) no history of myelofibrosis or acute myeloid leukemia before the index date; 4) ≥2 HCT measurements since the index date, and 5) no phlebotomy or hydroxyurea therapy before the index date. The outcome was the time from the index date to the first TE or to the last day of follow-up for censored cases.
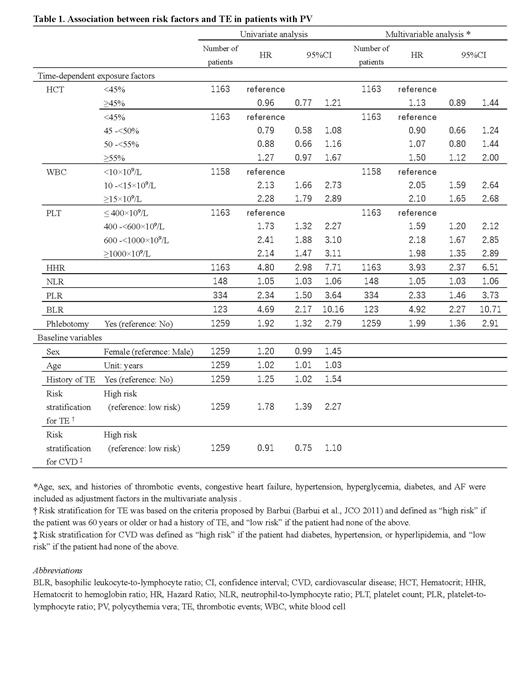
The primary analysis evaluated the association between HCT and TE using a univariate time-dependent Cox proportional hazards (PH) model. In the secondary analysis, WBC, platelet count (PLT), hematocrit-to-hemoglobin ratio (HHR), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), basophil-to-lymphocyte ratio (BLR), phlebotomy were used as time-dependent exposures, whereas age, sex, risk factors for cardiovascular disease, and Barbui's risk stratification were used as baseline variables to evaluate their associations with TE. A multivariable-adjusted Cox PH model with each time-dependent exposure and baseline variables was also conducted.
Results: Of 1,796 patients diagnosed with PV, 1,259 met the eligibility criteria. The median age (interquartile range [IQR]) of the patients was 66 (55-74) years; 63.1% were male; 23.1% had a history of TE; 71.9% were in the high-risk group according to Barbui's stratification; and 37.5% had one or more comorbidities (diabetes mellitus, hypertension, or dyslipidemia). The median (IQR) follow-up period was 1.3 (0.1-4.6) years.
Of the 1259 patients, 45.0% (566) developed TE during the follow-up period and the incidence rate was 14.4 (95% confidence interval [CI], 13.2-15.6) per 100 person-years. The median HCT at the time of the first TE was 49.5% (HCT <45%: 157 [32.4%], ≥45%: 328 [ 67.6%]); the median WBC and PLT were 10.2×10 9/L and 335.0×10 9/L, respectively.
In the primary analysis, the hazard ratio (HR) and 95% CI for TE in patients with HCT ≥45% compared with patients with HCT <45% was 0.96 (0.77-1.21), with no significant association. Age, history of TE and Barbui's risk stratification were associated with the risk of TE (HR [95% CI]: 1.02 [1.01-1.03], 1.25 [1.02-1.54], 1.78 [1.39-2.27], respectively). Compared with patients with WBC <10×10 9/L, patients with WBC ≥15×10 9/L and 10-≤15×10 9/L were associated with an increased TE risk (multivariable-adjusted HR [95% CI]: 2.10 [1.65-2.68] and 2.05 [1.59-2.64], respectively). Compared with patients with PLT <400×10 9/L, patients with PLT ≥1000×10 9/L, 600-<1000×10 9/L, and 400-<600×10 9/L were associated with an increased TE risk (multivariable-adjusted HR [95% CI]: 1.98 [1.35-2.89], 2.18 [1.67-2.85], and 1.59 [1.20-2.12], respectively). High HHR, NLR, PLR, BLR values and phlebotomy were associated with an increased TE risk (multivariable-adjusted HR [95% CI]: 3.93 [2.37-6.51], 1.05 [1.03-1.06], 2.33 [1.46-3.73], 4.92 [2.27-10.71] and 1.99 [1.36-2.91]).
Conclusions: This is the largest and first real-world cohort study to demonstrate the association between blood cell counts and TE in Japanese patients with PV. The results did not show that maintaining an HCT <45% is associated with a reduced risk of TE in Japanese patients with PV. In contrast, the risk of TE was associated with phlebotomy, Barbui's risk stratification, and elevated WBC, PLT, HHR, PLR, and BLR. These data support the need to consider blood cell counts other than HCT in treatment strategies for Japanese patients with PV in clinical practice. Furthermore, follow-up studies are required to identify the specific levels of blood cell counts associated with an increased TE risk.
Disclosures
Yasunaga:Novartis: Honoraria; Boehringer Ingelheim: Honoraria; Eli Lily: Honoraria; Chugai: Honoraria; Tsumura: Honoraria. Sugimoto:Pfizer Japan Inc.: Honoraria; Takeda Pharmaceuticals Co., LTD.: Honoraria; Kyowa Kirin Co., Ltd.: Honoraria; AbbVie GK.: Honoraria; PharmaEssentia Japan: Honoraria; Incyte Biosciences Japan GK: Research Funding; Toyo Kohan., LTD: Research Funding; Novartis: Honoraria. Uenaka:Novartis: Other: Novartis provided funds to RWD K.K., and I received my salary from RWD K.K., Research Funding. Dochi:Novartis Pharma K.K.: Current Employment. Jun:Novartis Pharma K.K.: Current Employment.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal